It is time for our Monday medical report.
Psoriasis is the most common autoimmune disease in the United States, affecting as many as 7.5 million Americans. It is often misdiagnosed as a rash, ringworm or other skin irritation, such as eczema, according to the National Psoriasis Foundation.
About 30 percent of those who develop the skin disease also go on to develop psoriatic arthritis, an inflammatory form of arthritis that can be disabling.
Psoriasis is not generally thought of as life-threatening, but it just might be for those with the severest forms of the disease.
In a new study, people with severe psoriasis had a 50% increased risk of death compared with people without the inflammatory skin disease.
“A significant number of people with psoriasis have an increase in heart disease, strokes, and things like that. So it is pretty important if you have severe psoriasis that covers more than 10 percent of your body to check with your family doctor and make sure they are monitoring you for any heart disease type things,” said Dermatologist Dr. Beverly Held.
Psoriasis is a common skin condition that speeds up the life cycle of skin cells. It causes cells to build up rapidly on the surface of the skin.
“There is no cure for psoriasis as of today. But we have multiple treatments, depending on the severity of the psoriasis and how much of the body area is being covered. We can either use surface treatments: creams, lotions, potions, and things we rub on it. We can go all the way to new biologic treatments which are injectables,” said Dr, Held.
Psoriasis is a chronic disease that often comes and goes. The main goal of treatment is to stop the skin cells from growing so quickly.
“The skin disease can be managed with these newer treatments that we have, however, they are expensive and not all insurance will cover them. But most of the time, we can get the skin pretty clear,” said Dr. Held.
There is no cure for psoriasis, but you can manage symptoms. Lifestyle measures, such as moisturizing, quitting smoking and managing stress, may help.
“Most of the people who have psoriasis don’t have too many symptoms. They can be very itchy in some cases. So they may have a lot of itching, and a lot of patients find that it is really aggravating when they get under more stress,” said Dr. Held.
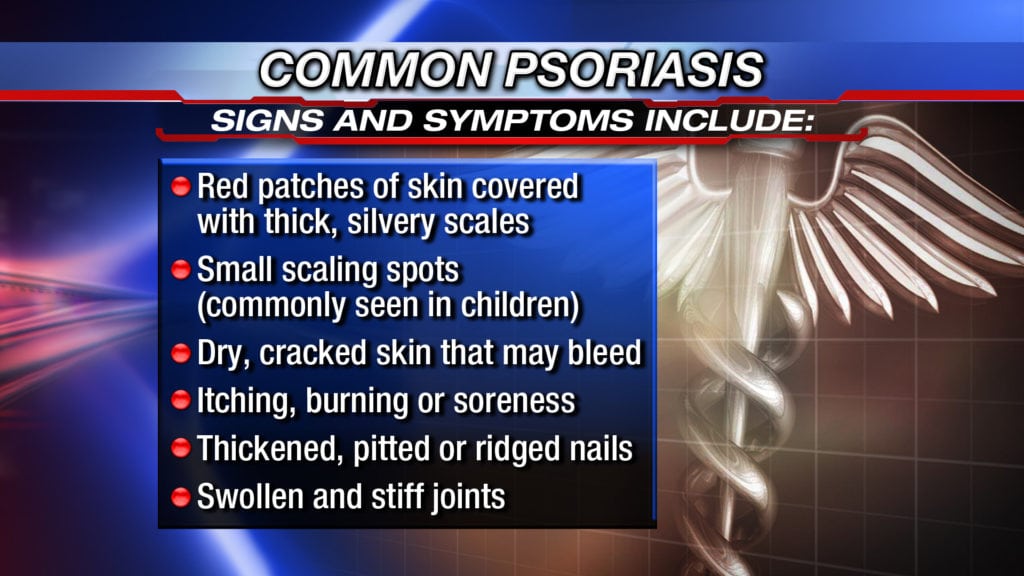
Symptoms
Psoriasis signs and symptoms are different for everyone. Common signs and symptoms include:
- Red patches of skin covered with thick, silvery scales
- Small scaling spots (commonly seen in children)
- Dry, cracked skin that may bleed
- Itching, burning or soreness
- Thickened, pitted or ridged nails
- Swollen and stiff joints
When to see a doctor
If you suspect that you may have psoriasis, see your doctor for an examination. Also, talk to your doctor if your psoriasis:
- Causes you discomfort and pain
- Makes performing routine tasks difficult
- Causes you concern about the appearance of your skin
- Leads to joint problems, such as pain, swelling or inability to perform daily tasks
Seek medical advice if your signs and symptoms worsen or don’t improve with treatment. You may need a different medication or a combination of treatments to manage the psoriasis.
Causes
The cause of psoriasis isn’t fully understood, but it’s thought to be related to an immune system problem with T cells and other white blood cells, called neutrophils, in your body.
T cells normally travel through the body to defend against foreign substances, such as viruses or bacteria.
But if you have psoriasis, the T cells attack healthy skin cells by mistake, as if to heal a wound or to fight an infection.
Overactive T cells also trigger increased production of healthy skin cells, more T cells and other white blood cells, especially neutrophils. These travel into the skin causing redness and sometimes pus in pustular lesions. Dilated blood vessels in psoriasis-affected areas create warmth and redness in the skin lesions.
The process becomes an ongoing cycle in which new skin cells move to the outermost layer of skin too quickly – in days rather than weeks.
Skin cells build up in thick, scaly patches on the skin’s surface, continuing until treatment stops the cycle.
Just what causes T cells to malfunction in people with psoriasis isn’t entirely clear. Researchers believe both genetics and environmental factors play a role.
Psoriasis triggers
Psoriasis typically starts or worsens because of a trigger that you may be able to identify and avoid. Factors that may trigger psoriasis include:
- Infections, such as strep throat or skin infections
- Injury to the skin, such as a cut or scrape, a bug bite, or a severe sunburn
- Stress
- Smoking
- Heavy alcohol consumption
- Vitamin D deficiency
- Certain medications – including lithium, which is prescribed for bipolar disorder, high blood pressure medications such as beta blockers, antimalarial drugs, and iodides
Risk factors
Anyone can develop psoriasis, but these factors can increase your risk of developing the disease:
- Family history. This is one of the most significant risk factors. Having one parent with psoriasis increases your risk of getting the disease, and having two parents with psoriasis increases your risk even more.
- Viral and bacterial infections. People with HIV are more likely to develop psoriasis than people with healthy immune systems are. Children and young adults with recurring infections, particularly strep throat, also may be at increased risk.
- Stress. Because stress can impact your immune system, high stress levels may increase your risk of psoriasis.
- Obesity. Excess weight increases the risk of psoriasis. Lesions (plaques) associated with all types of psoriasis often develop in skin creases and folds.
- Smoking. Smoking tobacco not only increases your risk of psoriasis but also may increase the severity of the disease. Smoking may also play a role in the initial development of the disease.
Complications
If you have psoriasis, you’re at greater risk of developing certain diseases. These include:
Psoriatic arthritis. This complication of psoriasis can cause joint damage and a loss of function in some joints, which can be debilitating.
Eye conditions. Certain eye disorders – such as conjunctivitis, blepharitis and uveitis – are more common in people with psoriasis.
Obesity. People with psoriasis, especially those with more severe disease, are more likely to be obese. It’s not clear how these diseases are linked, however. The inflammation linked to obesity may play a role in the development of psoriasis. Or it may be that people with psoriasis are more likely to gain weight, possibly because they’re less active because of their psoriasis.
Type 2 diabetes. The risk of type 2 diabetes rises in people with psoriasis. The more severe the psoriasis, the greater the likelihood of type 2 diabetes.
High blood pressure. The odds of having high blood pressure are higher for people with psoriasis.
Cardiovascular disease. For people with psoriasis, the risk of cardiovascular disease is twice as high as it is for those without the disease. Psoriasis and some treatments also increase the risk of irregular heartbeat, stroke, high cholesterol and atherosclerosis.
Metabolic syndrome. This cluster of conditions – including high blood pressure, elevated insulin levels and abnormal cholesterol levels – increases your risk of heart disease.
Other autoimmune diseases. Celiac disease, sclerosis and the inflammatory bowel disease called Crohn’s disease are more likely to strike people with psoriasis.
Parkinson’s disease. This chronic neurological condition is more likely to occur in people with psoriasis.
Kidney disease. Moderate to severe psoriasis has been linked to a higher risk of kidney disease.
Emotional problems. Psoriasis can also affect your quality of life. Psoriasis is associated with low self-esteem and depression. You may also withdraw socially.